Radiology
What is Onco-Radiology?
Onco-Radiology is a specialized branch of radiology focused on cancer care. It involves use of advanced imaging techniques to detect, diagnose, stage, and monitor cancers. These imaging tools are vital for identifying tumors early, guiding treatment decisions, evaluating response to therapy, and providing palliative care when needed.
The imaging modalities used in onco-radiology include:
Digital X-rays
Ultrasound with Elastography
Mammography and 3D Tomosynthesis
CT Scans (Computed Tomography)
MRI (Magnetic Resonance Imaging)
Each modality plays a unique role in helping clinicians visualize different tissues and organ systems to ensure comprehensive cancer management.
Our Services
1. Cancer Diagnosis and Staging
Early detection leads to better outcomes. Our department offers high-resolution imaging for accurate diagnosis and staging of cancers. Depending on the type and location of the tumor, we use:
X-rays for initial detection of abnormalities
Mammography and Tomosynthesis (3D Mammography) for early breast cancer detection
Ultrasound and Ultrasound Elastography to distinguish benign from malignant lesions
CT Scans for cross-sectional imaging of tumors in the chest, abdomen, pelvis, and brain
Each patient’s diagnostic plan is tailored to ensure optimal accuracy, minimal discomfort, and timely results.
2. Interventional Radiology
Our Interventional Radiology unit offers minimally invasive, image-guided procedures that aid in diagnosis and sometimes treatment. These include:
Biopsy and FNAC (Fine Needle Aspiration Cytology): Guided procedures to collect tissue from suspicious lesions. We are the only centre in the region offering stereotactic biopsy, a precision technique particularly useful in breast cancer.
Marker Placement: Radiopaque markers are placed to aid in future tumor identification and surgical planning.
Fluid Aspirations: Guided drainage or sampling of fluid collections (pleural, ascitic, cystic) to relieve symptoms and support diagnosis.
Drainage Catheter Placement: Image guided drainage of collections from various body sites in abdomen and thorax are carried out using ultrasound or CT scan guidance and help in minimally invasive management of many difficult clinical situations.
All procedures are performed under strict aseptic conditions with ultrasound or CT guidance for maximum accuracy and patient safety.
3. Monitoring and Follow-Up
Cancer treatment doesn’t stop at diagnosis. Imaging is crucial in:
Monitoring tumor shrinkage or stability during chemotherapy or radiotherapy
Detecting recurrence or metastasis
Assessing post-surgical healing and complications
We schedule regular imaging reviews as part of each patient’s personalized follow-up protocol to support long-term outcomes.


Why Choose Us?
At Andromeda Cancer Hospital, our Onco-Radiology Department stands out for the following reasons:
Expert Radiologists: Our team includes radiologists with extensive oncology-specific experience, ensuring the highest diagnostic accuracy.
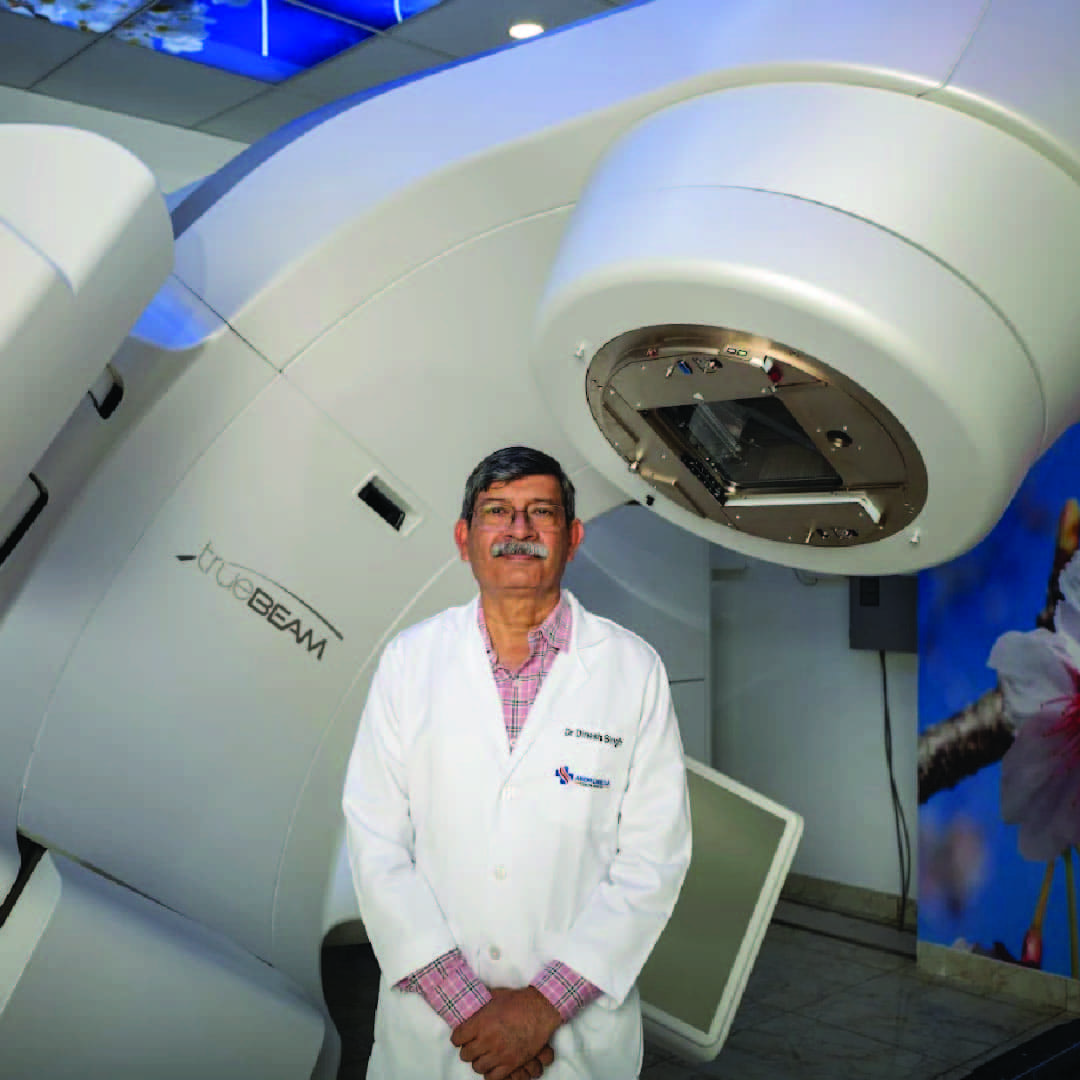
State-of-the-Art Technology: We use the latest imaging systems that deliver high-resolution results with minimal radiation exposure and faster scan times.
Tailored, Patient-Centric Care: Every patient’s journey is different. We personalize imaging strategies based on clinical needs, comfort, and urgency.
Integrated Cancer Care: Our radiologists work closely with surgical, medical, and radiation oncologists as part of a multidisciplinary cancer team to ensure coordinated care.
Our Technology
We are equipped with advanced imaging systems to ensure precision in every scan: Digital X-ray systems with low-dose radiation output. We have fixed as well as portable x-ray systems. Both systems are fully digital. Native digital systems reduce radiation dose and improve image quality. Ultrasound machines both in room and portable with multiple probes (sector, linear and intracavitary) with elastography. High quality ultrasound equipment, advanced algorithms for image management and skilled radiologists lead to high quality results. Full Field Digital Mammography with Tomosynthesis (3D Mammography) for enhanced detection of early-stage breast cancers Multislice CT scanner for high-speed, high-resolution cross-sectional imaging Image-guided biopsy systems, including stereotactic platform for pinpoint accuracy These technologies allow us to detect even small or complex lesions and provide real-time support during cancer interventions.
PACS and RIS at Andromeda Cancer Hospital
The onco-radiology department at Andromeda Cancer Hospital has a state-of-the-art IT system with two essential digital tools—PACS (Picture Archiving and Communication System) and RIS (Radiology Information System). These systems play a vital role in delivering efficient and accurate cancer care.
PACS (Picture Archiving and Communication System)
PACS is used to store, retrieve, view, and share medical imaging files such as X-rays, CT scans, MRIs, PET-CT, and mammograms.
Advantages of PACS in Oncology:
Centralized image storage – All scans are stored digitally and accessed instantly from any workstation.
Faster diagnosis – Quick access to images helps radiologists and oncologists make timely decisions.
Comparative review – Enables easy comparison of current and past scans for treatment monitoring.
Multidisciplinary access – Surgeons, oncologists, and radiation oncologists can view scans during tumor board discussions.
RIS (Radiology Information System)
RIS manages patient data, scheduling, imaging orders, and reports within the radiology department.
Advantages of RIS in Oncology:
Streamlined scheduling – Efficient appointment booking and patient tracking
Accurate documentation – Tracks imaging requests, scan reports, and patient history
Faster reporting – Helps generate and deliver radiology reports quickly to the treating team
Data management – Supports audits, quality control, and cancer registry inputs
Together, PACS and RIS improve the speed, accuracy, and coordination of cancer imaging services—making cancer diagnosis, staging, and treatment planning more effective and patient-focused.
Patient Care and Support
We understand that undergoing scans or procedures for cancer can be stressful. That’s why we’ve created a supportive environment where patients feel informed, safe, and cared for.
Consultations with Radiologists: Before or after procedures, patients can discuss the process, safety, and findings directly with our team.
Patient Education: Clear, easy-to-understand explanations of procedures, preparation steps, and expected outcomes are provided.
Emotional Support: Our radiology team works closely with counsellors and care coordinators to provide psychological support and ease patient anxiety.

Conclusion
At Andromeda Cancer Hospital, our Onco-Radiology Department is more than just an imaging unit—it is a cornerstone of comprehensive cancer care. By combining state-of-the-art technology with expert clinical insight and compassionate support, we ensure that every scan, procedure, and follow-up contributes meaningfully to a patient’s healing journey. From early detection to precise interventions and continuous monitoring, we are committed to delivering timely, accurate, and patient-focused radiology services that empower both clinicians and patients in the fight against cancer.
FAQs
Q. Is radiation therapy painful?
No, radiation therapy itself is painless. You won’t feel, see, or hear the radiation beam during treatment—it's similar to getting an X-ray.
Q. How many sessions will I need?
The number of sessions (fractions) varies depending on the cancer type, location, and purpose of treatment. It can range from a single session (as in SBRT or SRS) to 5–35 sessions for conventional treatments.
Q. What side effects should I expect?
Side effects depend on the area being treated and may include fatigue, skin redness, soreness, or changes in bowel/bladder habits. Most side effects are temporary and manageable.
Q. Is it safe to be around family after radiation?
Yes. External beam radiation (like TrueBeamSTx) does not make you radioactive. It’s perfectly safe to be around family, including children and pregnant women.
Q. How does stereotactic radiation differ from conventional therapy?
Stereotactic radiation (SRS/SBRT) delivers very high doses of radiation in a few precise sessions using sub-millimeter accuracy. Conventional therapy delivers smaller doses over more sessions and is used for larger or more complex targets.
Q. Will radiation affect my ability to work or do daily activities?
Many patients continue with light work and daily routines during treatment. Fatigue may build up over time, but rest and hydration help manage it.
Q. Can I eat normally during radiation therapy?
Yes, unless advised otherwise. In some cancers (like head & neck or gastrointestinal), dietary adjustments may be needed to manage side effects.
Q. Will I lose hair from radiation?
Hair loss only occurs in the area being treated. For example, radiation to the brain may cause scalp hair loss, but chest radiation will not.
Q. Is radiation therapy safe for older adults or those with other health problems?
Yes. Radiotherapy is commonly and safely used in elderly patients and those with comorbidities. Each plan is tailored to the patient’s health status.
Q. How is my position kept the same every day?
We use custom immobilization devices and daily imaging to ensure you are positioned accurately during every treatment session.
Q. Will radiation therapy cure my cancer?
In many early-stage cancers, radiation alone or in combination with other treatments can be curative. In advanced stages, it can help control disease and relieve symptoms.
Q. What is Deep Inspiratory Breath Hold (DIBH), and why is it used?
DIBH is a technique used during left-sided breast cancer treatment. It protects the heart by increasing the distance between the heart and breast during radiation.
Q. What is Image-Guided Radiation Therapy (IGRT)?
IGRT uses imaging before or during treatment to ensure accurate targeting of the tumor. It improves precision and safety by adapting to daily anatomical changes.
Q. Will I need to stay in the hospital during radiation?
Most radiation treatments are outpatient procedures. You can go home the same day unless other treatments or conditions require hospital admission.
Q. How do I prepare for my first radiation session?
You’ll have a planning session (simulation), and our team will explain the process, position you properly, and provide instructions. Wear comfortable clothing and follow any specific guidelines given.
