Breast
Oncology
Recognizing the importance of breast cancer in terms of the rising number of cases, the existing burden of the disease in the Indian population and the increasing complexity of breast cancer treatment, Andromeda Cancer Hospital has developed a centre of excellence for breast cancer management. This centre of excellence is called “Andromeda Breast Cancer Centre”. It has a multi-disciplinary team of dedicated breast cancer specialists and other healthcare professionals who provide state-of-the-art diagnostic facilities, personalized treatment and long-term care to every patient.
Andromeda Breast Cancer Centre
Setting Benchmarks of Excellence in Breast Cancer Care
Andromeda Breast Cancer Centre offers comprehensive facilities with the latest technology for the diagnosis and management of breast cancer.
OPD consultation for all breast-related ailments
- Outpatient clinic with patient-friendly and pleasant atmosphere
- Excellent team of patient navigators
Diagnostic facilities for all breast-related problems
- 3-D full-field digital mammography (tomosynthesis)
- High-resolution ultrasound with elastography
- All image-guided breast interventions and breast tumour localization facilities
- Stereotactic breast biopsy with comfortable biopsy chair
- Whole body PET CT scan
Multidisciplinary team
- Oncoplastic breast surgeons
- Medical Oncologists
- Radiation Oncologists
- Radiologists/Interventional Radiologists
- Pathologists
- Pain and Palliative Care Specialists
- Clinical Psychologists
- Breast Care Nurses
Treatment Facilities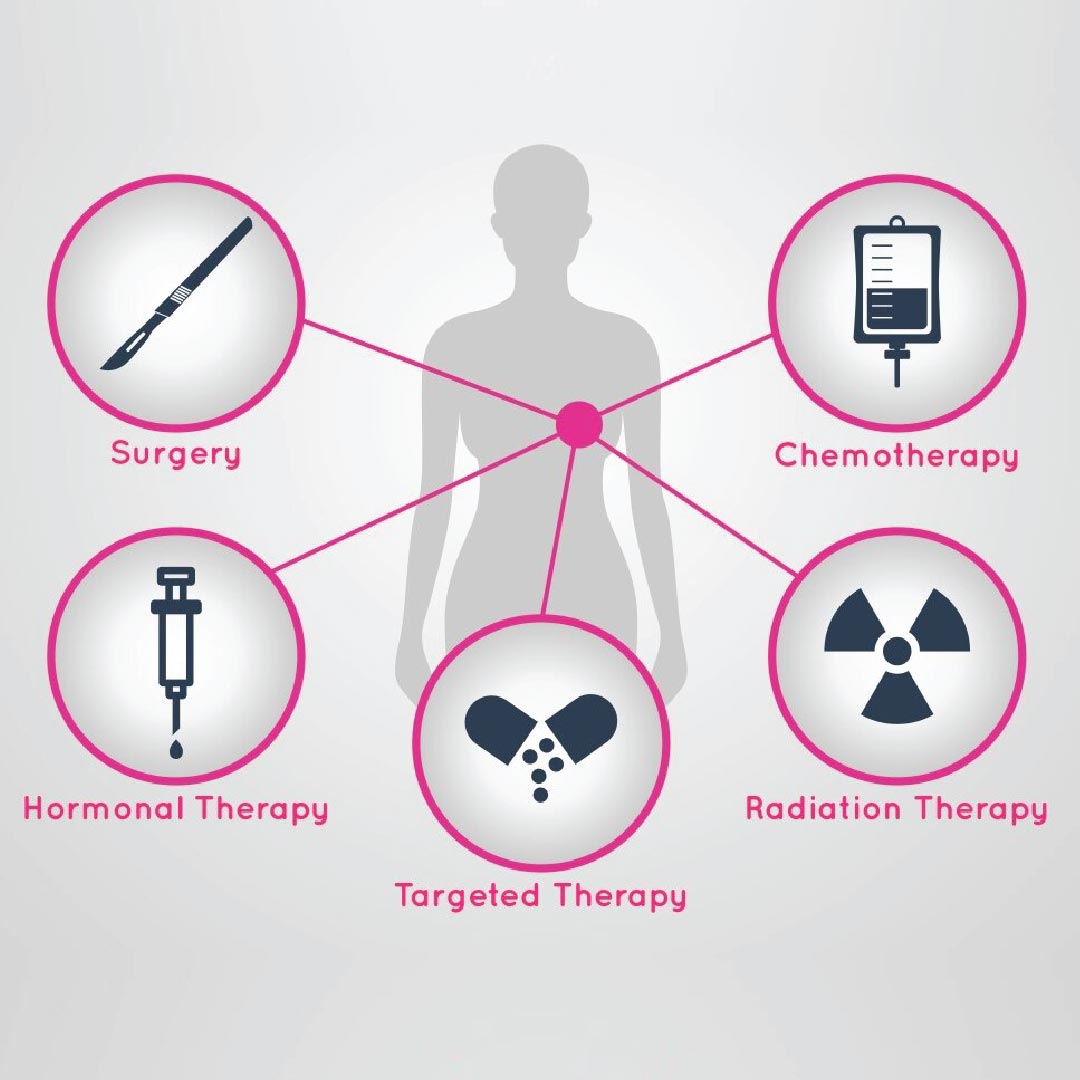
We offer personalized treatment for individual breast cancer patients through multi-disciplinary discussions based on international management guidelines.
Modern breast cancer surgery (with intraoperative frozen section facility)
- Well-equipped major and minor operation theatres
- Breast Conservation Surgeries
- Oncoplastic Breast Surgeries
- Modified Radical and Conservative Mastectomies
- Whole Breast Reconstruction (Primary and secondary)
- Sentinel Node Biopsy (Dual tracer technique)
- Long term vascular access (Chemo port/PICC line)

Advanced Drug Therapy For Breast Cancer
A fully equipped chemo-daycare facility
- Chemotherapy
- Immunotherapy
- Targeted therapy
- Endocrine therapy (Hormone therapy)
State of the art radiation therapy with TrueBeamSTx
- IMRT
- IGRT
- Deep inspiratory breath hold (DIBH)
- Conventional fractionation and Hypofractionation
- Respiratory gating
- Heart and lung-sparing
Facilities for holistic management and personalized wellness of breast cancer patients
- Genetic counselling and testing
- Breast cancer screening
- Fertility preservation counselling for young patients
- Psychological counselling
- Nutritional counselling
- Breast Cancer Support Group
- Advanced molecular services
- DEXA scan and bone health monitoring
- Vascular access for chemotherapy (Venous ports and PICC lines)
- Physiotherapy, lymphedema clinic and Rehabilitation
- Hair accessories, external breast prosthesis
- Pain management and palliative care services
Why Andromeda Breast Cancer Centre?
- Equipped with state-of-the-art technology to provide complete breast cancer care facilities under one roof
- Availability of all the latest equipment and expertise needed for the diagnosis, staging and treatment helps the patient in avoiding delays in the initiation of treatment.
- Integrated, muti-disciplinary team approach to the treatment saves the patients and their loved ones from the inconvenience of running around from one place to the other during various phases of the treatment.
- Is managed by a team of experienced oncologists, expert breast radiologists and Pathologists, breast care nurses, female radiology technicians and support staff
- Offers the personalized breast treatment plan with Multi-Disciplinary Team approach
- Provides effective communication among the treating doctors to allow any modifications in the treatment, if required (based on individual patient’s needs)
Andromeda Breast Cancer Centre offers a one stop facility for the diagnosis and comprehensive management of breast cancer and other non-cancerous breast related ailments.
Breast Cancer: An overview
- It is the commonest cancer affecting women globally. Breast cancer affects men, too. The ratio of women: men with breast cancer diagnosis is 100:1.
- Modern breast cancer treatment facilities have significantly improved the outcome of the disease.
- Early detection, early initiation of treatment and quality care can improve survival of breast cancer patients.
- Regular screening and knowledge of early warning symptoms & signs are the two key factors which help in early detection.
- 5-year breast cancer survival is now excellent at 95%, 92% and 70% for stage I, II and III respectively
Breast Cancer Scenario in India:
- In India, annually, nearly 30% of all cancer patients (more than 2 lakh) are women affected by breast cancer.
- Breast cancer is diagnosed a decade earlier
- There are many factors responsible for this changing trend, the young population structure being one of them
- Breast cancer is commonly diagnosed in stage 2 and 3, rarely in stage 1
- The proportion of women with aggressive biology is higher compared to the west
- Lack of awareness and comprehensive diagnostic/treatment facilities are responsible for the delay in diagnosis
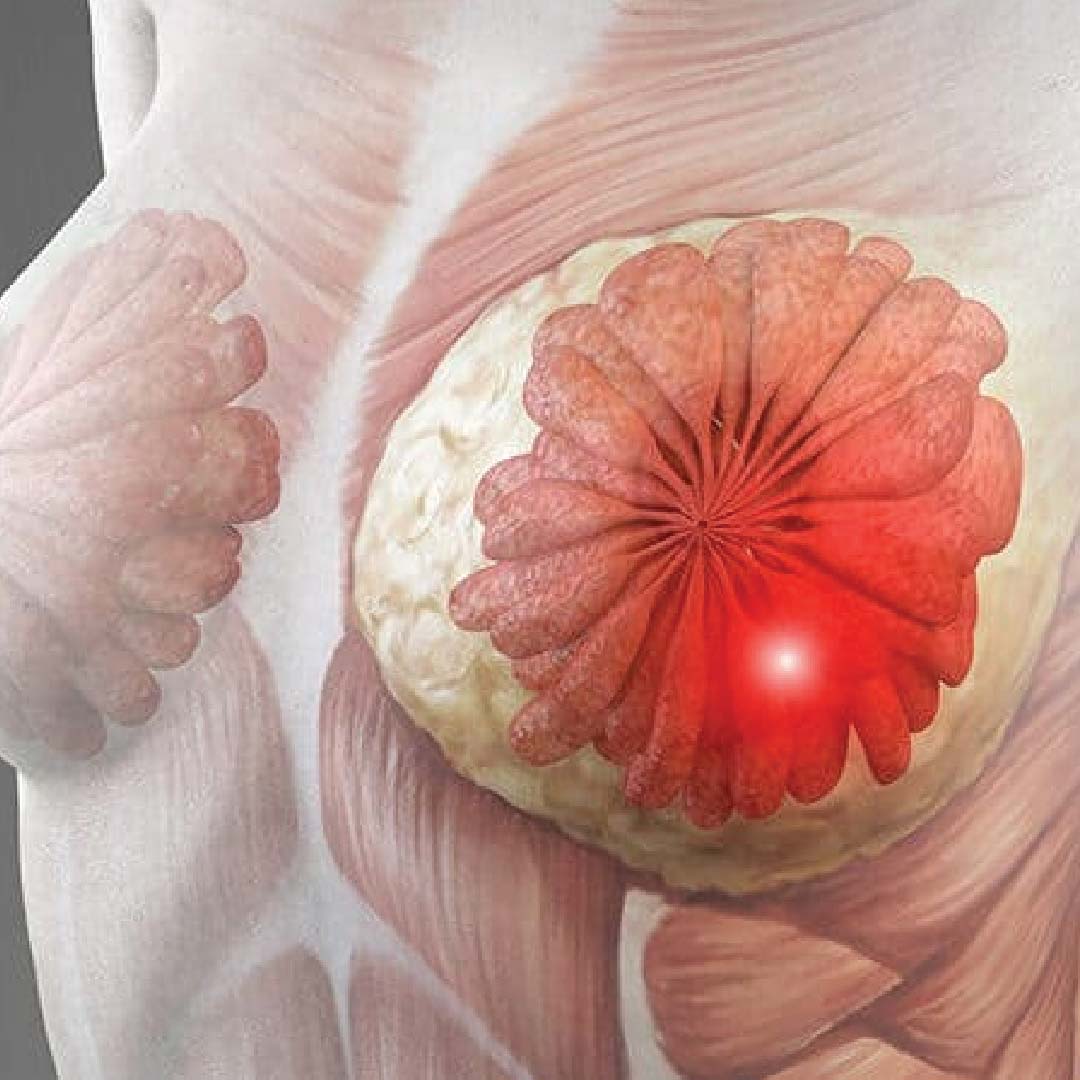
How does Breast Cancer Develop?
A normal cell(s) of the breast tissue gets converted into an abnormal cancerous cell due to an abnormality in the DNA of the breast cell(s). These abnormal cells continue to multiply in number. Accumulation of such abnormal cells can take the form of a firm to hard lump or distort tissues inside the breast. The cancerous process can either start within the cells of milk ducts (lactiferous ducts) or milk glands (lactiferous glands or lobules). Rarely, the cancerous process can start in any part of the breast like fat or connective tissue.

What are the different types of breast cancer?
There are two main groups of breast cancer
- Non-invasive or in situ breast cancer: (Ductal/Lobular Carcinoma in Situ)
- When the abnormal cells remain within the confines of the ducts or lobules, it is labelled as non-invasive or in-situ cancer. This type of cancer does not tend to spread inside the breast or to other parts of the body.
- Invasive breast cancer: (Invasive Ductal/Lobular Carcinoma)
- Occasionally a cancerous lump in the breast can have both invasive and non-invasive components together.
- There are many other less common types of breast cancer

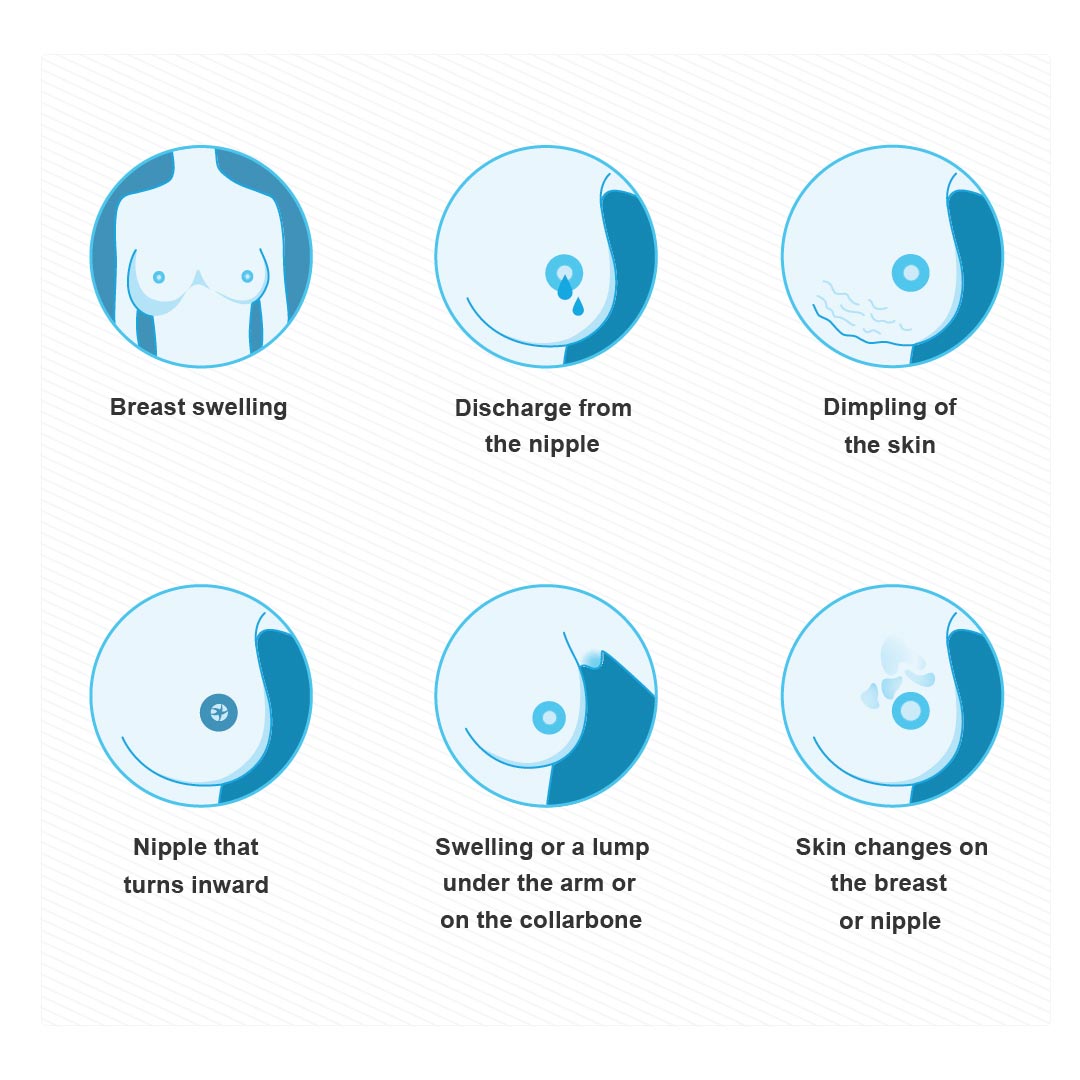
What are the common symptoms and signs of breast cancer?
A painless lump in the breast: It is the most common sign of breast cancer. While most of the lumps or masses are not cancers, please consult a breast specialist if you notice any lump in your breast. The chance that a new lump over the age of 40 years being cancer is higher than in a young lady in her twenties and thirties. But, regardless of age, any lump in the breast should be investigated.
Other symptoms and signs of breast cancer can include
- Swelling of a part or of the entire breast (even when a lump is not felt)
- Skin dimpling
- Orange peel appearance of the breast skin
- Nipple turning inwards (nipple retraction)
- Nipple discharge
- Rash on nipple or breast skin (red, dry, flaky, thickened)
- Swollen lymph nodes under the armpit or near the collarbone
Oncoplastic breast surgeries:
Breast conservation surgery initially had strict criteria. It was considered unsuitable for patients with large tumours or challenging locations. Conventional breast conservation surgery causes breast distortion in such cases. Oncoplastic techniques, blending plastic and cancer surgery, have expanded its scope. We can now remove a larger volume of the breast yet restore the cosmetic shape with oncoplastic techniques. These techniques involve reshaping surrounding tissue or using additional tissue to fill surgical cavities.
Based on this oncoplastic breast surgeries are grouped as
- Volume displacement procedures
- Volume replacement procedures
Based on the complexity of the procedure, oncoplastic surgeries are graded as Type I, II, and III, requiring specialized training. Procedures vary by tumour location and may involve the opposite breast for symmetry. Therapeutic mammoplasty reduces large, drooping breasts, improving radiation delivery, reducing complications, and relieving shoulder and neck strain.
Modern Radiation therapy for breast cancer:
Radiotherapy is an integral part of the loco-regional treatment of breast cancer. Radiotherapy helps reduce the recurrence of the disease in the breast (after breast conservation surgery) and chest wall (after mastectomy, complete removal of the breast). It has also been to improve overall survival. All patients who undergo breast conservation surgery need radiotherapy regardless of the pathological stage (except for a few very old patients with hormone receptor-positive breast cancer) Patients with pathologically positive lymph nodes and larger tumours may need radiotherapy even after mastectomy. The radiation field also covers the areas of neck nodes and nodes inside the upper part of the chest (Internal mammary chain nodes) for patients who have a high risk of recurrence. Radiation treatment nowadays is meticulously planned on planning CT scans and delivered with daily imaging conformations of the planned areas. Modern radiation delivery techniques (IMRT, IGRT, DIBH) have led to a significant reduction i
Can breast cancer be prevented?
There is no sure way to prevent breast cancer. There are no preventive vaccines available. The risk factors like age, being born a female, personal and family history, and inherited gene mutations cannot be modified.
However, one can reduce the risk of developing breast cancer by following measures:
- Maintaining healthy weight
- Using a balanced diet (low fat, low sugar, high fibre diet)
- Avoiding or limiting the use of alcohol
- Doing regular physical activity
- Avoiding unsupervised use of hormone pills containing estrogen
- Understanding your risk of breast cancer and discussing risk-reducing strategies
What are the risk factors for breast cancer?
The factors which increase one’s risk of developing breast cancer can be divided into two groups;
Non-modifiable actors: Some of the important non-modifiable factors are:
- Sex: Being a female is one of the strongest risk factors for breast cancer. Males can also get breast cancer, but it is much more common in females.
- Age: Breast cancer is usually seen in older women (commonest between 45-70 years). However, breast cancer is on the rise in young women these days. In our country, the average age of patients getting breast cancer is a decade earlier than the western counterparts.
- Starting menstrual periods early and having late menopause: A person who starts having menstrual periods quite early in life (say at the age of 9-10 years) and continues to have regular periods beyond the age of 50 years, has a higher risk of breast cancer.
- Personal history of breast cancer: A woman is diagnosed with breast cancer on one side, has a higher risk of developing cancer in the opposite breast, especially if the person is a carrier of high-risk genetic mutations like BRCA 1 and 2.
- Family history: Having one or more close blood relatives (mother/father, sibling, child, aunt, grandparent), who had breast, ovarian or any other related cancer increases the risk of breast cancer development in that person. It is important to know that only 15-20% of breast cancer patients have any significant family history.
- Nearly 80-85% of breast cancer patients develop breast cancer without having any such family history.
- Inheriting genetic mutations: An inherited mutation in genes like BRCA 1 & 2 can significantly increase the risk of breast cancer
- Having radiation to the chest at a young age: Women treated with radiation therapy to the chest before the age of 30 years have a much higher risk of breast cancer.
- Having dense breast tissue: Women whose breasts appear denser on mammograms are at a higher risk of breast cancer.
Dense breast tissue can also make it harder to see cancer on mammograms.
Modifiable risk factors: The following lifestyle-related factors increase the risk of breast cancer
- Drinking alcohol
- Excess body weight, especially weight gain after menopause
- No being physically active
- Taking hormone replacement therapy containing estrogen for a long time after menopause
- Not having children or having a first child after the age of 30 years
- Prolonged use of estrogen-containing birth control pills

Why is it important to get diagnosed at an early stage of breast cancer?
Early diagnosis is key to increasing survival rates and improving the quality of life for the women affected with breast cancer.
- Increased Survival Rates: When breast cancer is detected at an early stage, the five-year survival rate is nearly 100%. Early-stage cancers are usually smaller and have not spread, making them easier to treat successfully.
- More Treatment Options: Early detection provides patients with a broader range of treatment options, including less extensive surgeries like breast conservation, sentinel node biopsy etc. This reduces the risk of complications and improves the quality of life. Some patients with early stage of breast cancer (especially hormone receptor-positive cancers) may even avoid chemotherapy, leading to fewer side effects and a quicker recovery.
- Improved treatment outcome: The earlier cancer is found, the less likely it is to have spread to other parts of the body. This translates to a better prognosis and a higher likelihood of a complete cure.
- Reduced cost of the treatment:Treating cancer at an early stage is generally less expensive than treating advanced cancer, which can require more complex and prolonged treatment.

How is breast cancer diagnosed:
The diagnosis of breast cancer is always done by “Triple assessment”.
- Examination of the breasts by the clinician
- Radiological assessment of the breasts
- Pathological assessment of the abnormal area (Biopsy)
Patients presenting with suspicious breast symptoms and clinical signs need to undergo the following steps;
Step No 1: This includes an assessment of clinical history related to the breast symptoms and a thorough clinical examination of both breasts, armpits and neck.
Step No. 2: Any suspicious finding during clinical examination needs further radiological investigation such as mammography (women above 40), ultrasound scan (women below 40), and/ or MRI of both breasts. Occasionally, all may be needed.
Step No. 3: This is the most important step in breast cancer diagnosis.
- FNAC (fine needle aspiration cytology): Faster and easier to perform and gives quicker results but is less accurate
- CNB (Core needle biopsy): It is the gold standard for pathological assessment of suspicious breast changes. Ultrasound-guided core needle biopsy is the most ideal, simplest, accurate and economical way of performing this procedure.
- It can be done without USG guidance if the lump is large. Abnormalities that cannot be seen on USG scan are biopsied under mammography or stereotactic guidance) and those that are seen only on MRI need biopsy under MRI guidance. But this is rarely needed.
- USG-guided Fine Needle Aspiration Cytology (FNAC) or core needle biopsy (CNB) of nodes in the armpit is also a part of the pre-treatment investigation for breast cancer.
Staging workup: After the diagnosis of breast cancer is confirmed, it is important to assess the stage of the disease before deciding on the treatment plan.
The staging process includes the assessment of disease has spread to any other part of the body like the lungs, liver, bones or brain. The tests may vary depending on the patient’s symptoms indicating the spread of the disease. The likelihood of the spread of the disease to other parts of the body is very minimal in early-stage disease; hence only x ray chest and an ultrasound scan of the abdomen suffice. For locally advanced diseases or for patients with
A whole-body PET CT scan is advised for:
- Locally advanced disease
- Suspicious symptoms suggesting advanced disease
- Suspicious findings in baseline investigations

How can breast cancer be diagnosed early?
1. Empowerment through awareness:
Knowledge about breast cancer, the risk factors, the early signs and symptoms of the disease is the first step towards early diagnosis which empowers women to seek prompt consultation and get diagnosed early.
2. Breast Cancer Screening:
Screening is a process to look for cancer in people who do not have any symptoms. Mammography, the best tool for breast cancer screening, is usually recommended once in 2-3 years after the age of 40-45 years for women with an average risk of breast cancer. For younger women with a high risk of breast cancer (due to family history or inherited genetic abnormalities), a combination of mammography, high-resolution ultrasound scan and contrast-enhanced MRI of the breasts helps in early detection.
3. Triple assessment:
For early diagnosis of breast cancer, suspecting breast cancer and doing high-quality testing is part of a process called “triple assessment” which consists of clinical assessment by a specialist, imaging (mammography and/or ultrasound) and pathological testing (image-guided core needle biopsy).

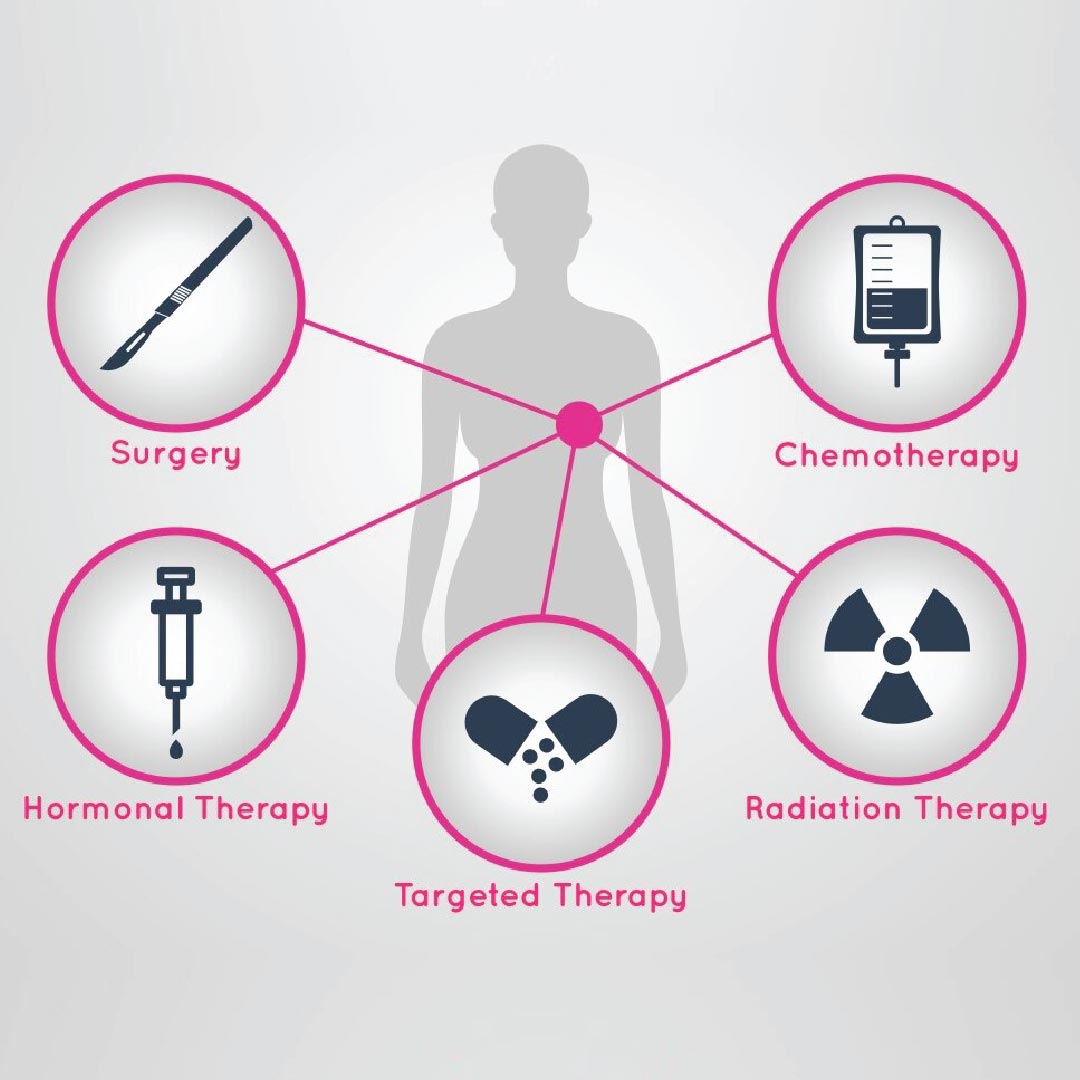
How is breast cancer treated?
Over the last few decades, we've learned that breast cancer is not a single disease but has many subtypes, each behaving differently.
Treatment is best delivered by a multi-disciplinary team and is personalised. Three important components of treatment are:
- Surgery
- Systemic therapy (Chemotherapy/Targeted therapy/Immunotherapy/Hormone therapy)
- Radiation therapy
Following are the factors taken into consideration before planning the treatment for an individual with breast cancer
- Age
- Stage of the disease
- Height/Weight/Body Mass Index (BMI)
- Breast cancer biology (Receptor status like ER/PR/Her 2 neu/Ki 67)
- Other medical conditions like, hypertension, diabetes, heart disease, asthma, etc.
- Patient’s wish
In addition to the cancer treatment, restoring the patient’s quality of life is a priority. Alongside oncologists, physiotherapists, dieticians, breast care nurses, psychologists, and radiation physicists work to provide comprehensive and holistic care. Not every patient requires every treatment modality. The treatment plans are personalized, ensuring that each individual receives tailored, effective care.
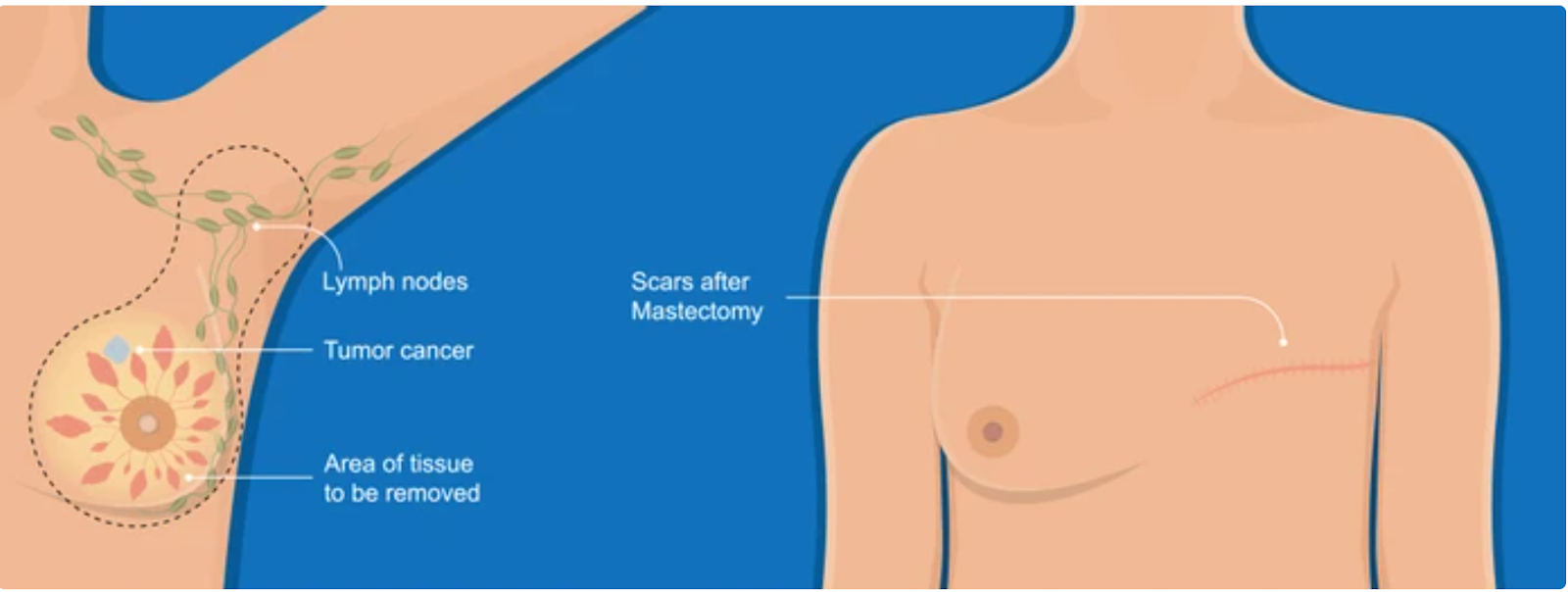
Surgery for breast cancer:
There are two main components of breast cancer surgery:
- Removal of the cancerous part of the breast
- Removal of armpit lymph nodes
Removal of the cancerous part of the breast:
It can be achieved by removal of the entire breast (called as mastectomy) if a large part of the breast is involved at the time of the diagnosis or by removal of only a part of the breast if the extent of the disease in the breast is limited (called as breast conservation surgery).
Mastectomy:
It involves the removal of the entire breast on the affected side, a part of skin overlying the tumour, nipple-areola and armpit lymph nodes. This leads to a flat horizontally placed scar on the chest.
The following types of mastectomies are performed for breast cancer
- Conventional modified radical mastectomy
- Conservative mastectomy
- Skin-sparing mastectomy: Entire skin on the breast is conserved, only the nipple and areola are removed with the breast
- Nipple (Nipple and areola) sparing mastectomy: Almost the entire skin and nipple and areola are conserved, only the breast is removed.
Conservative mastectomy is suitable for patients with tumours away from the skin and nipple areola. It is done along with immediate breast reconstruction
Breast Conservation Surgery (Lumpectomy/Quadrantectomy/Wide local excision)
Breast conservation surgery is a safe surgical option for selected patients.
The primary goals of breast conservation surgery are:
- Complete removal of breast cancer with clear margins
- To maintain the cosmetic shape and contour of the operated breast
Breast conservation surgery includes the removal of the cancerous lump in the breast with a margin of healthy tissue all around it and the removal of lymph nodes in the armpit through the same cut or a separate cut depending on the location of the tumour.
Breast conservation therapy (BCT) includes breast conservation surgery + radiotherapy to the whole breast. Unless the patient is very old, all patients who undergo breast conservation surgery need radiation therapy.
Breast conservation has also been proven to improve body image issues, psychological health and quality of life of women with breast cancer.
Breast reconstruction:
Patients who undergo mastectomy (removal of the entire breast) because of the advanced local stage of the disease or by choice can undergo breast reconstruction surgery. In this procedure, the shape and contour of the breast can be rebuilt using either the patient’s own tissue (Autologous flap-based) or using an implant. This procedure can be done at the same time as mastectomy (immediate reconstruction) or at some time (delayed reconstruction).
Autologous flap-based reconstruction:
In this procedure with the help of advanced microvascular techniques and patient’s tissue from various donor sites, natural, soft breast mounds, can be created, considering individual needs and health conditions.
Implant-based breast reconstruction:
Implant-based breast reconstruction can be performed in single-stage or two-stage. Today, a variety of implants can be chosen to match the opposite breast. This type of breast reconstruction may carry a risk of implant rupture and additional corrective surgeries.
Removal of axillary lymph nodes:
Breast cancer can spread to armpit lymph nodes. Removal of armpit lymph nodes is required to determine the disease stage and guide treatment.
Following surgical procedures are performed for the removal of axillary lymph nodes:
- Complete axillary lymph node dissection/clearance (ALND)
- Sentinel lymph node biopsy (SLNB)
Previously, all armpit nodes of the affected side were removed, causing complications like arm swelling, shoulder stiffness, and numbness. Many early-stage patients without node involvement underwent unnecessary overtreatment. We now use a more selective approach for patients who have early disease. Recently, a few studies have also concluded that patients with low risk of disease recurrence may be operated on without any surgery for armpit nodes.
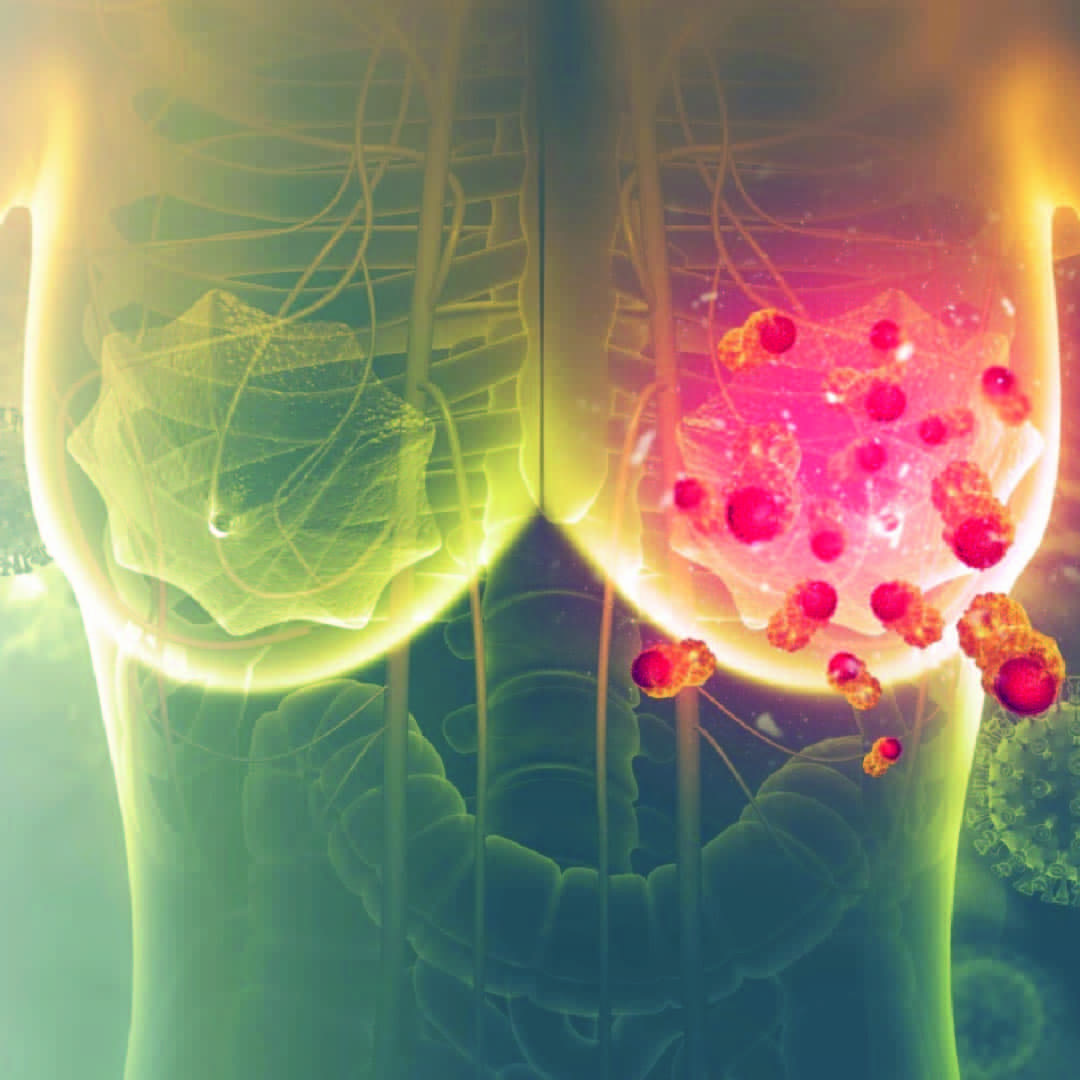
Advanced systemic therapy for breast cancer (Chemotherapy, Immunotherapy and Targeted therapy and Hormone therapy)
Systemic therapy is an important part of the multidisciplinary management of breast cancer in all stages. The use of systemic therapy in the management of breast cancer has helped in improving survival or improve quality of life.
Systemic therapy is used sequentially with surgery and radiation therapy in stage I, II, III. For stage IV (metastatic stage) of breast cancer, sometimes only systemic therapy is used. Most patients with early-stage breast cancer are treated with loco-regional treatment in the form of surgery and radiation while chemotherapy is contemplated to control micrometastatic disease and prevent recurrences. However, all early breast cancers may not require chemotherapy.
Breast cancer is not a single disease. Based on the appearance of the cancer cells under the microscope and disease biology, breast cancer can be classified into many different subtypes. These subtypes behave differently and require different treatment approaches.
Modern systemic therapy for breast cancer involves using medications that travel throughout the body to target the cancer cells. These therapies include:
- Chemotherapy: It uses drugs to kill fast-growing cancer cells. Patients with high-risk diseases are treated with a combination of drugs (called as cytotoxic chemotherapy drugs). The use of chemotherapy reduces the risk of disease coming back significantly. Chemotherapy can be administered before surgery (Neoadjuvant chemotherapy) or after surgery (Adjuvant chemotherapy). The doses and interval between each chemotherapy session depend on the breast cancer subtype and tolerance of the patient. Today, patients tolerate chemotherapy much better because of the availability of many new drugs which help in reducing the side effects.
- Hormone therapy: It consists of oral tablets or injections that block the hormones (like estrogen) that can drive the growth of certain types of cancer cells. It is advised when the breast cancer cells express Estrogen (ER) and/or Progesterone receptors (PR). For stage I, II, and III, hormone receptor-positive breast cancers, patients are advised oral hormone therapy tablets for 5-10 years after completion of the treatment.
- Targeted therapy: Patients with Her 2 positive subtypes of breast cancer are treated with Her 2 targeted therapy which blocks the HER2 protein, helping to slow cancer growth and improve treatment outcomes for patients. Most of these drugs are available in the form of injections (Trastuzumab, Pertuzumab, TDM1, TDXd, etc). Lapatinib is one such medicine that can be taken in the form of oral tablets. These drugs are used along with chemotherapy drugs (in the adjuvant as well as neoadjuvant setting) and later on (after completion of all chemotherapy) in the form of a single injection or a combination of two Her 2 targeted injections every 3 weeks for 1 year.
- Immunotherapy: Immunotherapy for breast cancer is the newer exciting option of drugs that boost the body’s immune system to recognize and attack cancer cells, offering a promising treatment option for certain breast cancer types. These drugs, used alone or along with chemotherapy have been found to improve survival rates and quality of life in selected patients with breast cancer (depending on breast cancer subtype and stage).
- Novel oral therapies for breast cancer: With the ongoing research in the medical field, newer agents are being added to the treatment armamentarium every year increasing the chances of survival and responses. These new additions include drugs like Cyclin-dependent kinase (CDK) inhibitors, PIK3CA inhibitors, small molecule tyrosine kinase inhibitors but also various injectable molecules in the form of monoclonal antibodies and antibody-drug conjugates.
Today, most of the patients with hormone negative (ER/PR/Her 2 neu negative, triple negative) and Her 2 positive breast cancers are treated with chemotherapy first followed by surgery. In some triple-negative subsets of breast cancer addition of immunotherapy (Pembrolizumab) has significantly improved the outcome of cancer treatment. However, in a country like India, these modern systemic therapy options remain unaffordable for the majority of the population.
Conclusion
Andromeda Breast Cancer Centre is redefining breast cancer care in India with a blend of cutting-edge technology, expert multidisciplinary teams, and personalized patient care. Early detection, holistic treatment, and integrated support services make it a true centre of excellence.
FAQs
Q. What is breast cancer surgery?
Breast cancer surgery involves removal of the cancerous tissue from the breast. It may range from breast-conserving surgery (lumpectomy) to complete removal of the breast (mastectomy), depending on the stage and type of cancer.
Q. What are the different types of breast cancer surgeries?
The main types include:
- Lumpectomy: Removal of only the cancerous lump with surrounding tissue.
- Mastectomy: Removal of the entire breast.
- Sentinel lymph node biopsy (SLNB): Removal of first few lymph nodes for checking spread.
- Axillary lymph node dissection (ALND): Removal of multiple lymph nodes if cancer has spread.
- Reconstructive surgery: Rebuilding the breast shape after mastectomy.
Q. How do doctors decide which surgery is best for me?
Your surgeon considers the tumor size, stage, breast size, genetic factors, and personal preferences. The goal is to remove cancer completely while preserving appearance and function as much as possible.
Q. What is breast-conserving surgery and who can have it?
Breast-conserving surgery (lumpectomy or wide local excision) removes only the tumour with a margin of healthy tissue. It is suitable for most early-stage cancers, usually followed by radiation therapy. However, patients with large tumours can be down staged with primary chemotherapy and offered breast conservation surgery.
Q. What is a sentinel lymph node biopsy and why is it done?
The sentinel lymph node is the first node to which cancer cells are likely to spread. This procedure helps to determine whether cancer has reached the lymph nodes, guiding further treatment while avoiding unnecessary extensive surgery.
Q. Is breast reconstruction possible after mastectomy?
Yes. Breast reconstruction can be done immediately during mastectomy or later after other treatments are complete. Options include implant-based or autologous tissue-based reconstruction (using one’s own body tissue).
Q. Will I need radiation or chemotherapy after surgery?
That depends on the stage, type, and biological behaviour of your cancer. After surgery, your oncologist reviews the biopsy report to decide if radiation, chemotherapy, hormonal, or targeted therapy is needed.
Q. How long does recovery take after breast cancer surgery?
Recovery varies with the type of surgery. Most patients return to routine activities in 2–4 weeks after breast cancer surgery.
Q. Will breast cancer surgery cause pain or swelling in the arm?
Some patients experience temporary pain, stiffness, or swelling (lymphedema). Early arm exercises and physiotherapy help prevent and control these symptoms effectively.
Q. Will I lose my entire breast if I have breast cancer?
Not always. Many women can undergo breast-conserving surgery, especially when the cancer is detected early. Even if mastectomy is required, reconstruction options can help restore breast shape.
Q. Can breast cancer come back after surgery?
There is a small chance of recurrence depending on cancer stage and biology. Regular follow-up visits, imaging, and medications (like hormone therapy) help reduce this risk and detect any recurrence early.
Q. Are both breasts removed to prevent future cancer?
Usually, no. Removing the healthy breast (preventive mastectomy) is only advised for women with strong genetic risk (e.g., BRCA mutation) or significant family history.
Q. How safe is breast cancer surgery?
Modern breast cancer surgery is very safe when performed by experienced surgical oncologists. Complications are rare and include bleeding, infection, or wound healing issues, all of which are manageable.
Q. How soon after surgery can I start my normal activities?
You can begin light activities like walking within a few days. Lifting heavy weights or strenuous exercise should be avoided for 3–4 weeks or until your surgeon advises.
Q. How often do I need to follow up after surgery?
Typically, follow-up visits are scheduled every 3 months for the first 2 years, and then every 6 months for next 3 years and then annually. These visits include physical exams, imaging, and review of your recovery and ongoing treatment.
